Coping with the Nursing Shortage: Strategies for Hospital CEOs
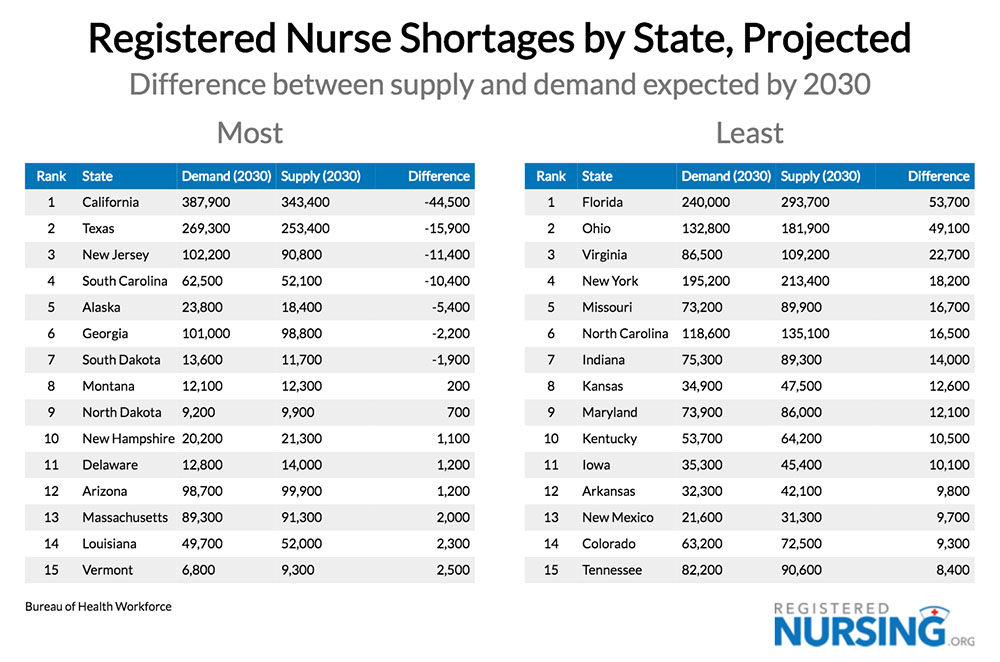
The nursing shortage has been an issue in the healthcare field for decades, but the situation has been growing increasingly dire in recent years. With an aging population and an increasing demand for healthcare services, many hospitals, particularly rural ones, are struggling to cope with this shortage and meet the needs of their patients. The severity of the shortage varies by state, as the following table from RegisteredNursing.org shows:
The Causes of the Nursing Shortage
The nursing shortage is caused by several factors. One of these factors is an aging population which consumes more health care resources as it ages. The median age of the U.S. population has risen almost nine years since 1980. The U.S. population aging trend has accelerated in recent years bringing with it an increase in rates of chronic issues like obesity and diabetes.
Another factor is the decline in the number of nursing school graduates, driven at least in part by the perception of better working conditions and more lucrative pay in other fields. The Covid-19 pandemic was a difficult time for the medical profession in general and particularly nurses. Even with the relative return to normalcy in recent months, the turnover rate among nurses remains high and has a significant impact on hospitals. According to the 2022 Nursing Solutions, Inc. (NSI) National Healthcare Retention and Staffing Report, the national average RN turnover rate in 2021 was 27%. The report further finds that each percent change in this turnover rate costs or saves the average hospital an additional $262,300 per year.
These factors have created a perfect storm in the nursing profession where many nurses are overworked and less willing to work overtime. Combine these conditions with the fact that many nurses also feel underpaid and undervalued, leading to a lack of motivation. These conditions lead to burnout, further increasing turnover.
Strategies for Coping with the Nursing Shortage
Hospital CEOs can take several steps to address the nursing shortage. The first is to increase salaries for nurses to make the profession more attractive. Additionally, improving benefits, such as offering tuition reimbursement for nurses who want to pursue advanced degrees, can help to retain nurses.
Hospitals should also focus on recruiting and retaining nurses from diverse backgrounds, as this can help to create a more inclusive and diverse workplace. Additionally, hospitals should strive to create a positive work environment for nurses that is focused on teamwork and collaboration.
Finally, hospitals should focus on improving nurse scheduling to ensure that nurses are not overworked and that they have adequate time for rest and relaxation. This can help to reduce burnout and improve morale.
What About Growth?
As hospital CEOs look for ways to cope with the nursing shortage, growth may be the furthest from their minds. How can any hospital grow amidst a shortage of the very personnel necessary for adding or expanding services? There is a way, and it’s through adding service lines that actually ease the burden on existing nursing staff.
Through the years and decades, more and more responsibilities have been placed on the shoulders of the nursing staff. In addition to caring for patients, they must also deal with a series of administrative tasks and serve as the communication focal point for care between patients, doctors, families, insurance, and drug companies. These additional responsibilities take time away from caring for patients. “I became a nurse so I could do paperwork,” said no nurse ever. Their passion is caring for patients.
Growth can occur, even during this nursing shortage, by adding service lines that remove the ancillary responsibilities that have crept into the nursing job description. A good example of this is outpatient IV infusion using the service model developed by Community Infusion Solutions. This model delegates the administrative tasks associated with the service — patient scheduling, insurance authorizations, communicating with referring doctors, etc. — to a case manager. All nurses must do in this service model is administer the IV therapy.
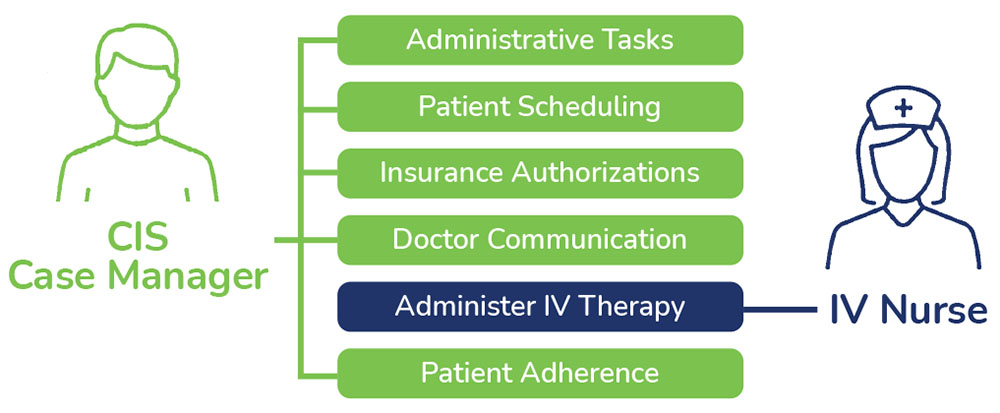
Mitchell Berenson, CEO of Community Infusion Solutions (CIS), has a unique perspective on adding service lines that don’t exacerbate the nursing shortage. Berenson regularly receives outpatient infusion therapy, and he also developed the CIS service model. “Our service model for outpatient IV infusions substitutes labor away from registered nurses. Most of our infusion programs are managed by LPNs at a fraction of the cost. My infusion nurse is not a registered nurse. She mixes the drugs and administers them, after providing phlebotomy. The nursing shortage does not connect to her, yet the local hospital earned $7,500 for the two hours I was there. That’s making something out of nothing in a nursing labor market full of holes.”
Conclusion
The nursing shortage is a complex and multifaceted issue that is not likely to be resolved quickly. However, hospital CEOs can take proactive steps to address the problem and ensure that their patients receive the best possible care. By increasing salaries, offering benefits, recruiting diverse nurses, and improving nurse scheduling, hospitals can begin to address the nursing shortage and ensure that their patients receive the care they need. Finally, even during this shortage, growth by adding or expanding services doesn’t have to be off the table. A service model that substitutes other labor for RNs, like the CIS model for infusion therapy, enables growth while relieving the burden on nurses.
