Leaving a Legacy by Building a Rural Oncology Program
At the start of his career, Mitchell Berenson had an experience which gave him a vision that would influence the course of his professional life. Working as a patient manager, he observed that oncology patients from rural areas had many pressing needs that were not being met. Getting necessary services was difficult. The solutions to their unmet needs could be found in a hospital that was hundreds of miles away, and the only connection to that hospital was by telephone.
Berenson, an NRHA fellow, founded and today leads Community Infusion Solutions (CIS), a turnkey public health solutions firm. CIS advocates for rural health by establishing a sustainable outpatient IV infusion service line. This service meets a need for the patient while increasing hospital revenue and patient access to care. Berenson’s experience with rural oncology patients remains a powerful influence on his work.
“Everybody gets cancer at about the same rate, but people in rural areas die of cancer at an increased rate than those in urban areas,” Berenson observed.
“In many cases, until a center of excellence level program is developed within that rural hospital and community, a lot of oncology patients are not going to get the care they need. I have seen patients that are wheelchair-bound who have become unemployed. They have communicated fear about being a burden on their families. This was hard for them because they are isolated living in their rural community.”
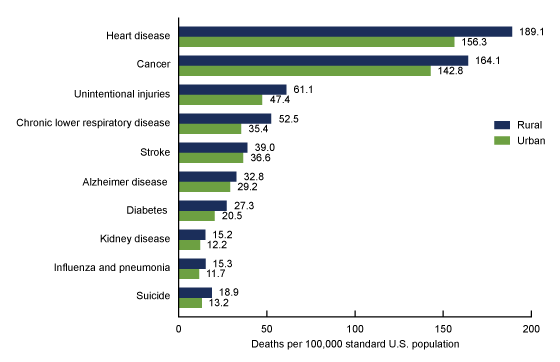
Source: National Center for Health Statistics.
Evidence from studies, including one done by the Centers for Disease Control, have confirmed that people in rural areas struggle more with cancer diagnoses and treatment, which is a factor leading to higher mortality rates. “The CDC study revealed that rural people are fatalists,” said Berenson. “They get a diagnosis and then they throw in the towel. From a public health standpoint, access to care is a barrier for rural oncology patients. Rural hospitals are delivering babies, replacing joints, and providing lots of care. But for some reason, many are not engaging in oncology.”
Berenson did his own research to understand why. On the surface, medical oncology seems a simple service for a hospital to provide. “I could see in the data that hospitals had the patients, but they had a problem serving those patients. The hospitals I talked to would acknowledge the need for these services. But there were extraneous factors that created reluctance for rural hospitals to provide medical oncology services.”
The Missing Piece: Psychosocial, Counseling, and Supportive Care
Gripped with a sense of urgency to do something about the lack of rural medical oncology services, Berenson conferred with Dr. Marcia Brand, who has served the rural population for decades through the Health Resources and Services Administration (HRSA), an agency of the US Department of Health and Human Services. There, she served as Deputy Administrator. Berenson and Brand’s joint conclusion was that what was missing was psychosocial programs, cancer counseling, and supportive care. “When a rural patient would get a cancer diagnosis, they didn’t have a toll-free number to call and ask questions, to learn about things like nutrition services,” said Berenson.
During this time, Berenson was asked to serve on the board of directors for the Cancer Support Community, a nationally recognized non-profit wholly focused on supportive care services for cancer patients. “When people get a cancer diagnosis, it’s overwhelming. Cancer Support Community becomes an ally for people with cancer by providing highly personalized, sustained support. This support is as important as the medical oncology drugs because it relates to how you feel about your cancer care. Is this something you’re going to survive? Do you have goals? When I looked at hospitals where Cancer Support Community was actively providing services, I found people were readmitted less to the hospital. The psychosocial support really works.”
Developing a Rural Oncology Program
Understanding all the key pieces of effective rural oncology is a good start. There is a two-stage process that rural hospitals can follow to successfully develop an oncology program.
Stage 1: Local Supportive Care
The first stage is the development of a local supportive care component. “We get the community involved as part of a grassroots activity,” Berenson states. “Our company helps by analyzing diagnosed cancer patients to determine frequency of types of cancer, such as prostate, breast, lung, colon, etc. to determine what is primary. We then work in the community to develop a board of directors to advise the cancer program. We do it this way because we don’t just want to stand up a program, we want to focus on sustainability. We want to ensure we are addressing the concerns of the people that have the fiduciary responsibility for that hospital.”
With a board in place that understands the community and its needs, what follows is creating a relationship with a regional hospital that provides access to medical oncology providers and radiation oncology providers. CIS creates and fosters a “narrow network” that allows a rural hospital to send its cancer patients to regional hospitals that collaborate with their local hospital. This approach lets the regional hospitals get the financial benefit of having a larger volume of patients, while at the same time, the rural hospital controls the quality of the care its referred patients are getting. “When we have that relationship with just one or two other organizations, we can case manage those patients through that supportive care component,” said Berenson.
Stage 2: Medical Oncology Program Development
The second stage is the actual development of a medical oncology program in the rural hospital. “There’s a lot of apprehension about where to start building a medical oncology program,” says Berenson. “After interviewing many people in the Federal Government, in rural America and in other places, we now know the best thing to do is to start with supportive care and then move to the medical oncology program. In Stage 1 of this process, you’ve already created a relationship with a bigger organization, the regional hub hospital. It’s then just a matter of getting those services back to the spoke hospitals, those rural hospitals.”
A barrier to Stage 2 is putting in place a medical oncology pharmacy that is compliant with current regulations. Most rural hospitals do not have this. “Our company will invest and pay for half of that development process,” Berenson states. “We will invest in the medical oncology program to get it up and going. And to ensure its success, we provide all the rest of the services an infusion program requires, such as marketing, case management services, and reporting activities. The CIS service model is a partnership with rural community hospitals to do all of these things. It’s a turnkey service.”
Opportunity is Significant but Fleeting
COVID showed how capable rural hospitals are in handling the increased severity of the patients they treat. “The goal for rural hospitals right now is to try to increase the severity index of all the patients that they’re caring for,” Berenson states. “If rural hospitals do not take advantage of this increased severity, this oncology revenue opportunity will go somewhere else. The healthcare industry will build cancer centers on the edge of urban settings and figure out a way around the ability of rural hospitals to take care of their own. Will those be comprehensive cancer programs? Absolutely not. The door is wide open at present for rural hospitals to build a medical oncology program, but it will not stay that way.”
Dr. Dean Walcott, a psychiatrist who is deeply involved in Cancer Support Community, shared his vision for comprehensive cancer care in rural America. It is not a singular focus on medical oncology at the drug level. It is holistic, considering the mind and the body of the patient. “Many cancer studies talk about the mind and the body, how you feel about what you’re going through,” Berenson concludes. “Rural hospitals are starting to realize they can play a major role in the cancer healing process. We are here to help them build successful oncology programs. As we talk to more hospitals and their boards, there is real excitement about how this can leave a legacy in their communities. I have witnessed excitement that is even bigger than putting your name on a new hospital building.”
Are you ready to expand your hospital's service lines with a turn-key solution? Complete the form below to request your free, no obligation Level 1 Analysis!
